Device development and commercialization requires a comprehensive approach that encompasses scientific rigor, innovation, regulatory compliance, and market readiness. With the increasing demand for advanced orthopedic solutions, it is crucial for organizations to adopt best practices to ensure successful device development from concept to commercialization. In this article, we explore the practices used in product development that can drive excellence in orthopedic development by accelerating time to market and delivering optimal patient outcomes.
1. MULTIDISCIPLINARY COLLABORATION:
By fostering a multidisciplinary approach, organizations can leverage diverse expertise, perspectives, and insights throughout the development process. Often, the best solution is provided by a new perspective. Successful orthopedic product development teams should include the following stakeholders: orthopedic surgeons (outside the ‘friends and family’ network), engineers, material scientists, industrial designers, regulatory experts, and market strategists. This collaboration enables the integration of clinical insights, engineering advancements, and market trends to create user-friendly devices that meet the needs of both patients and healthcare professionals.
2. HUMAN FACTORS ENGINEERING:
Integrating human factors engineering (HFE) into orthopedic device development is critical for ensuring usability, safety, and patient satisfaction. HFE focuses on optimizing the interaction between users and devices, considering factors such as ergonomics, user interfaces, and intuitive design. By conducting thorough user research, usability testing, and risk assessments, organizations can identify and address potential usability issues early in the development process, resulting in orthopedic instrumentation and implants that are intuitive, effective, and aligned with user needs.
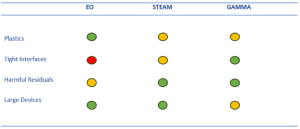
3. REGULATORY COMPLIANCE:
Orthopedic products are subject to stringent regulatory requirements to ensure patient safety and device effectiveness. Adhering to regulatory standards and engaging with regulatory authorities early in the development process is essential. By establishing a robust regulatory strategy, organizations can navigate the complex regulatory landscape, streamline the approval process, and accelerate time to market. Companies need to explore all regulatory avenues and not limit themselves to the 510(K) and take advantage of other regulations such as the FDA’s new De Novo process for unique claims and gain a competitive advantage. Compliance with regulations is crucial for successful commercialization and market access.
4. DESIGN FOR MANUFACTURING AND ASSEMBLY (DFMA):
Designing orthopedic devices with manufacturability and assembly in mind is a best practice that can enhance efficiency, reduce costs, and improve scalability. DFMA principles involve optimizing device design to minimize complexity, facilitate efficient manufacturing processes, and ensure consistency in quality. By collaborating closely with manufacturing partners early in the development process and incorporating DFMA considerations in prototypes, organizations can streamline production, minimize design iterations, and accelerate time to market.
5. POST-MARKET SURVEILANCE AND FEEDBACK:
Monitoring the performance and safety of orthopedic devices in real-world settings is crucial for continuous improvement and regulatory compliance. Establishing post-market surveillance programs to actively collect feedback from healthcare professionals and patients can provide valuable insights into device performance. Potential issues can be identified, and iterative enhancements will drive long term product life. This ongoing feedback loop helps organizations address any concerns, optimize device performance, and maintain regulatory compliance throughout the device lifecycle.
By embracing these best practices, organizations can enhance the development and commercialization of orthopedic devices, delivering solutions that improve patient outcomes and meet market demands. Multidisciplinary collaboration, human factors engineering, regulatory compliance, design for manufacturing and assembly, and post-market surveillance form a comprehensive framework for success in this evolving field. As the demand for innovative orthopedic solutions continues to grow, adopting these best practices is essential for organizations aiming to make a significant impact in the orthopedic device market and contribute to the advancement of patient care.
Back to Insights + News